Abstract
Introduction: β-thalassemias are rare genetic conditions characterized by mutations in the HBB gene, resulting in defective β-globin production and ineffective erythropoiesis. The severity of disease varies according to genotype. Periodic red blood cell transfusions (RBCTs) are the standard of care, but long-term dependence on RBCTs is associated with risk of iron overload and other clinical sequelae. As new treatment options are available, understanding the clinical burden of β-thalassemia and RBCTs is essential to optimal clinical care.
Methods: This retrospective observational study analyzed anonymized medical records from adults (≥ 23 years of age) with transfusion dependent β-thalassemia (TDT) or non-transfusion dependent β-thalassemia (NTDT) who visited a participating physician on or after January 2016. Physicians in the UK, France, Germany, Spain, and Canada abstracted medical records for eligible patients with ≥ 5 years of medical history in their practice. Clinical characteristics, transfusion patterns, and RBCT utilization were analyzed descriptively.
Results: A total of 214 patients were included: 118 (55%) with TDT and 96 (45%) with NTDT. Mean age was 36 years and body mass index was approximately 24 kg/m2 in both groups; 71% and 61% of patients with TDT and NTDT, respectively, were male. Mean (median) duration of patient medical history in the practice was 8.5 (7.5) and 8.6 (6.9) years for patients with TDT and NTDT, respectively.
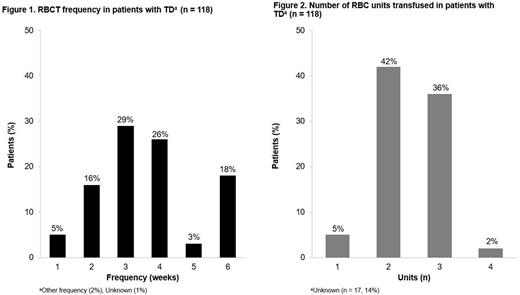
Among the TDT group, the mean (standard deviation [SD]) age at first diagnosis and first treatment of β-thalassemia was 11.1 (10.2) and 13.7 (11.2) years, respectively. The most common reasons for initiating RBCTs were: hemoglobin (Hb) levels < 8 g/dL (32%), < 7 g/dL (21%), < 6 g/dL (14%), and to maintain Hb > 10 g/dL (25%). The majority of patients (n = 87 [74%]) received β-thalassemia mutation testing; of these, 31 (36%) were β0/β0, 19 (22%) were β0/β+, and 23 (26%) were β+/β+. More than one-third (n = 41 [35%]) of patients with TDT had progressed from NTDT, at a mean (SD) age of 31.4 (11.7) years. The mean (SD) pre-transfusion Hb level in the TDT group was 6.9 g/dL (1.30) (n = 94). At the time of data abstraction, most patients with TDT (n = 90/118 [76%]) had an RBCT at least every 3 weeks (Figure 1), receiving a mean (SD) of 2.4 (0.64) RBC units (n = 101) per session. Approximately one-third (n = 43/118 [36%]) of patients with TDT received 3 RBC units per session, on average (Figure 2). Patients with TDT received their most recently reported RBCT regimen for a mean (SD) of 72.6 (72.43) months (n = 83). Adverse events (AEs) associated with the most recent transfusion regimen included allergic reactions (n = 3/118 [3%]), non-hemolytic febrile transfusion reactions (n = 2/118 [2%]), and transfusion-associated circulatory overload (n = 1/118 [1%]).
Among the NTDT group, the mean (SD) age at first diagnosis and first treatment of β-thalassemia was 14.5 (11.8) and 18.8 (12.0) years, respectively. Approximately two-thirds (n = 63 [66%]) of patients with NTDT received β-thalassemia mutation testing; of these, 7 (11%) were β0/β0, 19 (30%) were β0/β+, and 20 (32%) were β+/β+. Among patients with NTDT, who had ≥ 1 RBCT (n = 81 [84%]), the mean (SD) number of RBCTs received was 15.9 (15.88) (in the physician's practice or as history noted in the medical record). The most common reasons for receiving RBCTs were: Hb levels < 8 g/dL (33%), < 7 g/dL (20%), and < 6 g/dL (14%), infection exacerbating anemia (16%), and to maintain Hb > 10 g/dL (15%). The mean (SD) pre-transfusion Hb level was 7.4 g/dL (1.18) (n = 67) and a mean (SD) of 2.2 (0.57) RBC units (n = 66) was transfused per session. AEs for patients with NTDT included allergic reactions (n = 4/96 [5%]), alloimmunization (n = 1/96 [1%]), autoimmune hemolytic anemia (n = 1/96 [1%]), and nonhemolytic febrile transfusion reaction (n = 1/96 [1%]).
Conclusions: This study provides much needed insight into the real-world clinical needs of patients with β-thalassemia. About one-third of patients with TDT had progressed from NTDT. Patients with TDT had a high transfusion burden, requiring RBCTs every 2-4 weeks and 2-3 RBC units per session, on average. Additionally, patients with NTDT had low pre-transfusion Hb and required 2 RBC units per transfusion, on average. New therapeutic options are needed that can reduce RBCT dependency for patients with TDT, and improve pre-transfusion Hb levels and transfusion requirements for patients with NTDT.
Disclosures
Cappellini:Sanofi Genzyme: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Vertex: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Agios: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Silence: Membership on an entity's Board of Directors or advisory committees. Yucel:Bristol Myers Squibb: Current Employment, Current holder of stock options in a privately-held company. Meyers:Bristol Myers Squibb: Research Funding. Jimenez:Bristol Myers Squibb: Research Funding. Nham:Bristol Myers Squibb: Research Funding. Glassberg:BMS: Current Employment, Current holder of stock options in a privately-held company; Novartis: Ended employment in the past 24 months. Alashkar:German Research Foundation: Research Funding; Novartis: Consultancy, Honoraria; Agios: Consultancy, Honoraria; GBT: Consultancy, Honoraria; BMS/Celgene: Consultancy, Honoraria; University Hospital Essen: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.